The medical malpractice lawyers of Lupetin & Unatin are worried that doctors’ overconfidence in current screening protocols for Critical Congenital Heart Defects (CCHD) can lead to undiagnosed congenital heart defects in newborns. This overconfidence in CCHD screening is known to result in medical malpractice with devastating consequences.
Congenital heart defects cause more newborn deaths than any other type of congenital defect. Congenital heart defects represent nearly 40% of all deaths from congenital defects and 3% to 7½% of all infant deaths. About 25% of babies with a congenital heart defect (CHD) have a critical CHD. It is imperative that newborns born with a congenital heart defect are timely diagnosed as cardiac surgery has been shown to significantly improve survival especially for newborn babies with potentially life threatening congenital heart defects. If defects are not detected before the baby is discharged from the hospital, there is an increased risk of adverse complications in the future caused by the cardiac defect.
Ultrasonography conducted prior to the baby’s birth and meticulous newborn examination are critical to improving early diagnosis. In an effort to improve early detection rates, however, more and more hospitals are implementing screening of all newborns prior to hospital discharge with pulse oximetry. The rationale behind this is that many CCHD present with a degree of hypoxemia (oxygen deficiency) in the immediate neonatal period that would not necessarily be readily apparent to a doctor on clinical exam. CCHD pulse oximetry screening assists pediatricians and neonatologists in identifying babies born with congenital heart defects. Because of this, CCHD pulse oximetry screening is mandated in many states and common policy and procedure in most hospitals.
Pulse oximetry screening for CCHD has been studied extensively and thus its benefits as well as shortcomings are fairly well understood at this point. The data demonstrates that pulse oximetry screening is a highly specific test (99.9%) for detection of CCHD in asymptomatic newborn babies. It also has a low false positive rate (0.14%) which means that when a baby fails a CCHD pulse oximetry screen test, it is almost never a false alarm. Studies demonstrate, however, that the sensitivity of the pulse oximetry CCHD screening tests is a modest 76.5%. This means that of all babies born with a congenital heart defect, approximately 24% are not detected by pulse oximetry screening. Thus, while the pulse oximetry screening for CCHD is a highly specific test, it leaves much to be desired with respect to its sensitivity in detecting all congenital heart defects in newborns.
Studies have shown that there are seven (7) types of newborn congenital heart defects that are most often picked up by pulse oximetry screening. These lesions included hypoplastic left heart syndrome, transposition of the great arteries, pulmonary atresia with intact ventricular septum, tricuspid atresia, tetralogy of fallot, total anomalous pulmonary venous return, and truncus arteriosus.
What parents need to know is that pulse oximetry screening for CCHD has not been shown to detect heart defects like ventricular septal defects (VSD) that result in a left to right shunting of blood through the heart. A ventricular septal defect is a hole in the wall of the heart between the bottom two chambers. The septum is the wall that separates the left and right sides of the heart. VSDs shunt blood from left to right in the heart – exactly the type of defect that is not detected by CCHD pulse oximetry screening.
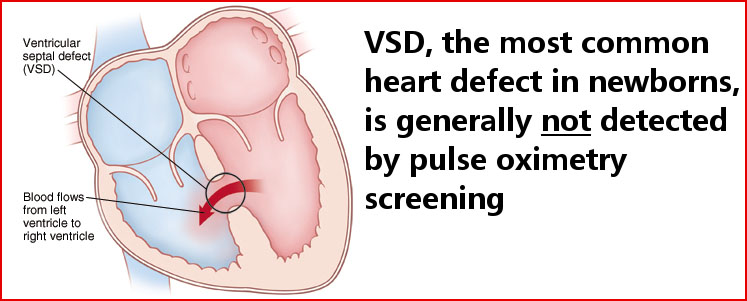
This is particularly concerning because VSD is the most common heart birth defect with approximately 1 in 500 babies born with the condition. Furthermore, 20% to 30% of all heart defects are isolated VSDs.
Despite the obvious benefits of pulse oximetry screening for CCHD there is a downside, which is the over confidence this test can instill in pediatricians and neonatologists. CCHD screening can lead some doctors to assume that all heart defects will be discovered even if a meticulous clinical exam is not performed. Relying predominantly on pulse oximetry screening is highly risky because the most common and in some cases the most devastating heart defect in babies, ventricular septal defect, is not detected by pulse oximetry screening. Because of this, most studies of pulse oximetry screening warn doctors that pulse oximetry screening cannot be relied on as the sole method for detection of CCHD. Clinical examination with a high suspicion of children born with heart murmurs is critical to detecting all heart defects.
Doctors that rely too heavily on pulse oximetry screening to identify congenital heart defects in newborns may be committing malpractice if they fail to undertake an adequate physical exam of the child.
There is no doubt that neonatal pulse oximetry screening results in significant improvement in the timely diagnosis of CCHD especially when conducted in combination with antenatal ultra-stenography and physical examination in the newborn phase. Newborn oximetry screening is an evidence-based program that has improved the detection of CCHD which in turn has led to improved outcomes for babies born with heart defects. Practitioners, however, must see this screening process for what it is – another net to catch defects at an early stage – and not a standalone test that obviates the need for in depth clinical evaluation.
If your child has been diagnosed with a congenital heart defect well after birth and is suffering serious complications as a result we urge you to contact our experienced medical malpractice attorneys.
