Every day, doctors and hospitals fight to save lives. Two of the fiercest enemies in this fight are sepsis and septic shock.
In plain terms, sepsis is a “a life-threatening condition that arises when the body’s response to an infection injures its own tissues and organs.” The CDC estimates that the number of people treated in the hospital for sepsis nearly doubled from 621,000 in the year 2000 to 1,141,000 in 2008. In addition, the CDC reports sepsis kills more than 258,000 Americans each year and is the ninth leading cause of disease-related death.
With the understanding that early recognition and treatment of such serious illness improves outcomes, an international task force of critical and intensive care physicians met in January 2014 to start the process of developing new definitions and more uniform criteria for the diagnosis of sepsis and septic shock. The results of their work, including the above definition of sepsis, were published last week in the Journal of the American Medical Association (JAMA).
Sepsis
Initially, the task force recognized there is no “gold standard” test for identifying sepsis. That said, doctors frequently suspect sepsis based upon the presence of two or more factors for the clinical syndrome known as Sudden Inflammatory Response Syndrome, or SIRS. The SIRS criteria includes abnormal temperature (>38 degrees Celsius or <36 degrees Celsius), elevated heart rate (>90 bpm), elevated respirations (>20 per min), and an abnormal white blood cell count or increase in the percentage of immature white blood cells (bands).
In the study titled “Assessment of Clinical Criteria for Sepsis”, the task force compared SIRS and other models for diagnosing sepsis to determine which method is most predictive of in-hospital deaths. Ultimately, they found the SIRS criteria is a very poor predictor of patients who will die due to sepsis, in part because its criteria includes signs and symptoms present in a vast number of patients who never develop sepsis or infection.
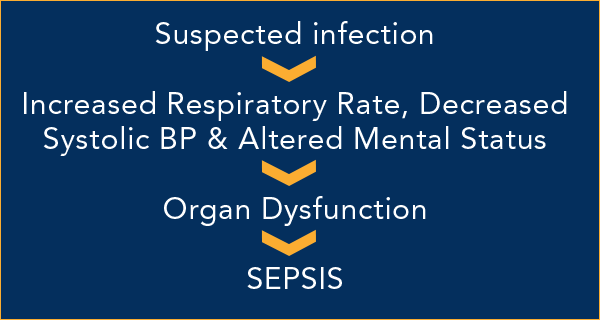
Recognizing the “increasing focus on early recognition of sepsis” for infected patients outside the ICU, the researchers focused on a new, “simple model” for the assessment of sepsis. The new model is known as “quick SOFA” or qSOFA for short, and uses three clinical measures: altered mental status, lower systolic blood pressure, and elevated respiratory rate.
The study found qSOFA was highly reliable for predicting hospital deaths from sepsis. In addition, the qSOFA model has the further benefit of expediency. The qSOFA criteria are based on information routinely recorded for patients in the hospital and, therefore should be readily available in a patient’s chart. No blood samples or lab results are required. And, qSOFA requires little in the way of calculations.
Ultimately, the task force recommended “qSOFA criteria be used to prompt clinicians to further investigate for organ dysfunction, to initiate or escalate therapy as appropriate, and to consider referral to critical care or increase the frequency of monitoring…”
Significantly, the failure to diagnose sepsis is too often preceded by the failure to diagnose an infection as a failure to diagnose sepsis itself. In recognition of this reality, the task force reminds the public “positive qSOFA criteria should also prompt consideration of possible infection in patients not previously recognized as infected.”
Septic Shock
Septic shock is now defined as “a subset of sepsis in which circulatory, cellular and metabolic abnormalities are associated with a greater risk of mortality than sepsis alone.” In practical terms, septic shock is the more deadly consequence of the progression of sepsis.
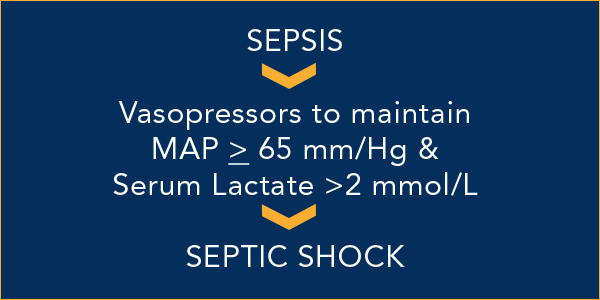
In the study titled “Developing a New Definition and Assessing New Clinical Criteria for Septic Shock”, the task force settled on two signs as the most important indicators of septic shock: hypotension and serum lactate. Hypotension is an abnormal decrease in blood pressure. For patients with sepsis, the body’s inflammatory response to severe infection can cause blood vessels to dilate. The widening of the vessels leads to decreasing blood pressure. Serum lactate is of one of the hallmarks cellular dysfunction. Elevated lactate in the blood indicates cells in the body are forced to convert nutrients into energy in the absence of much needed oxygen.
According to the study, the ideal clinical criteria for identifying septic shock in adult patients is now 1) hypotension requiring the use of vasopressors to maintain a mean blood pressure of 65 mm/Hg or greater and 2) a serum lactate level greater than 2 mmol/L which persists after a patient has received fluids.
In representing victims of medical malpractice, we often need to identify whether doctors overlooked or simply failed to interpret clear signs and symptoms of sepsis or septic shock. Inevitably, defendants and their experts muddy the waters and brush aside signs such as tachycardia, hypotension and low urine output as innocuous signs of a normal postoperative recovery or a myriad of other transient conditions insufficient to raise a red flag. With the diagnosis of sepsis, septic shock, or even infection dependent on such nonspecific signs and symptoms, we are often forced to focus instead on whether treaters failed to appreciate the underlying cause of infection, such as surgical injury to the bowel or bile duct,, a developing bone infection or even a slight wound of the skin.
We appreciate the task force’s desire and hard work to make this important step toward uniformity in the definition of sepsis and septic shock. Likewise, we hope the new criteria will help physicians solve the puzzle and give an opportunity for full recovery and life to the victims of sepsis and septic shock.
